Implanted Telescope Helps Patients Overcome Macular Degeneration
This file type includes high resolution graphics and schematics when applicable.
Age-related macular degeneration (AMD) is the leading cause of vision loss and affects 10 million Americans, more than those suffering from cataracts and glaucoma combined. That number could grow to over 20 million by 2020 as the U.S. aged population grows. Worldwide, the number afflicted in 2020 could be as high as 196 million.
There currently is no cure and doctors could do little more than prepare patients for the inevitable loss of vision in one or both eyes. Now, however, patients have an option, thanks to researchers at VisionCare who have developed an implantable telescope that can preserve a patient’s vision.
The Telescope
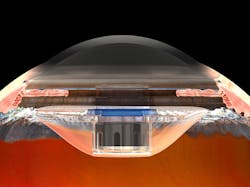
The implantable telescope consists of two lenses within a glass tube. It is about the size of a pencil eraser (3.6-mm in diameter and 4.4 mm) and uses bi-convex and bi-concave convergent and divergent micro-lenses coupled with air lenses, according to VisionCare. Details on the micro-optics are proprietary, but the outcome is that the implant acts like a fixed telephoto lens that works with the cornea to project images onto the retina that are enlarged by a factor of 2.7. The iris is also left in place, but the implant is longer than it is deep, so the end of the telescope protrudes through the inactive iris. Although the macula of the retina is partially destroyed and useless, the magnified image overlaps the diseased section to stimulate undamaged rods and cones to partially return central vision to the patient.
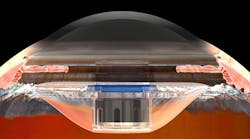
The implantable telescope from VisionCare improves the central vision of patients suffering from advanced macular degeneration. It gets implanted in one eye so that it can detect central vision (where the person is looking); the other eye then picks up the task of peripheral vision.
The implant also has a polymethylmethacrylate (PMMA) carrier and a blue PMMA restrictor. The sealed optical components snap-fits into the carrier, which includes shaped projections that hold the implant in place. These are similar to those found on intraocular lenses implanted in patients who have had cataract-removal surgery in which part of their natural lens is removed. The projections, called “haptics” by VisionCare, are snugged into the capsular bag, a smooth transparent membrane that surrounds the natural lens. Over time, the membrane grows up and around the haptics, securing the implant in place. But patients are still warned to avoid situations in which their head or eyes are exposed to trauma so they don’t damage or dislodge the implant. They are also told to refrain from rubbing their eyes too forcefully.
The blue-tinted restrictor, a washer-shaped component, surrounds the implant and reduces the amount of light that can enter the eye from the periphery so it does not wash out images coming in through the implant.
The optics are designed and built to have an optimal focusing distance of about 11.5 ft., assuming an average-sized eyeball. Patients are prescribed glasses if distance or near-viewing corrections are needed. There are no moving parts or electronics in the implant.
When implanted, the telescope is behind the undamaged cornea. The restrictor, the blue components, prevents too much light from entering around the edges of the telescope and washing out the image.
The device is implanted behind the iris in one eye during an outpatient surgical operation that also involves removing the eye’s natural lens. The implant is sterilized by the manufacturer using ethylene oxide (EtO). This gas infiltrates packaging and kills germs. EtO is often used on medical devices and components that need to be sterilized but cannot withstand conventional high-temperature steam sterilization. After sterilization, the implant is packaged and then not opened until inside the clean operating room.
Post-Op Results
After the operation, which usually lasts one to one-and-a-half hours, patients are given eye exercises and go through some training to get the most out of the implant. For example, they practice tracking objects with the new implant, as well as watching TV and reading. The exercises, which can last six to 12 weeks, also help reprogram the optical cortex of the brain and how it processes inputs from the eyes. This is needed because the patients are now using their eyes in a completely new way. In fact, vision gradually improves and it can take a few months before all the benefits are realized.
In post-op patients, the eye with the implant provided their brain with visual details of what they are looking directly at while the other eye provides peripheral vision. AMD does not affect peripheral vision, a low-resolution form of vision humans rely on for detecting objects near or nearing them and those moving in their field of vision. So instead of using two parts of the same eye, the patients (and their brains) need to switch between eyes to get the same information.
The implanted telescope sends visual information to areas outside the damaged macula (the dark red spot).
The implant has been shown to improve a person’s ability to identify what they are looking at, to “look” someone in the eye during conversation, and to see facial expressions. The implant can’t completely restore a person’s natural vision. However, in clinical tests, 50% of the people with the implant could read two to three lines lower on the standard eye chart, and 90% reported improved vision. Patients might also still require a magnifying glass to see fine details or small print.
The implant is practically unnoticeable to others because it is totally inside the eye and behind the iris, the colored portion of the eye.
The implant, which costs about $15,000, is approved by the FDA for patients 65 and older, and is covered by Medicare. It is designed to last the life of the patient.
The Threat: Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is an incurable eye disease that damages the macula, the small area near the center of the retina that contains a high concentration of light receptors (rods and cones). The macula is responsible for sharp, central vision and lets people see objects they are looking directly at.
This image simulates what a person with AMD sees: The central portion of the image is totally unusable, but the peripheral vision is still available (though blurry).
AMD is a slow-working disease and those with it might not notice any symptoms for years. Over time, however, the person’s center of vison in the affected eye(s) becomes increasingly blurry. The blurred spots grow and blind spots can develop in the eye’s field of vision over time. Eventually, central vision is lost altogether, rendering the person legally blind. They still might be able to see objects in their peripheral vision, but they can no longer read, see faces, drive safely, or do close work.
There are two types pf AMD, dry and wet. The dry version, which accounts for 90% of all AMD cases, results from the slow breakdown of light-sensitive cells in the retina and the supporting tissue beneath the macula. The other type, wet AMD, accounts for 10% of AMD patients, and is also known as late-stage AMD. In this stage, abnormal blood vessels grow underneath the macula. The vessels often leak fluids and blood, leading to swelling and damage to the macula. The damage is severe and happens quickly, unlike the slower pace of dry AMD. But not everyone who gets dry AMD develops wet AMD.
People with early AMD in only one eye have a 5% chance of developing late-stage AMD within 10 years. These with early AMD in both eyes run a 14% chance of developing late-stage AMD in at least one year after 10 years.
There is another form of macular degeneration called Stargardt disease. It is found in younger patients and is caused by a recessive gene. There is no cure for AMD, although high-dose vitamins and minerals and a healthy diet have been known to slow its progression. It’s also recommend that those with AMD stop smoking. (Smoking doubles the chances a person will contract AMD.)
Other risk factors for contracting AMD include genetics; AMD does run in families, but researchers have identified 20 genes that affect the risk of developing AMD, and many more are suspected. That’s why there are currently no genetic tests that reliably predict if someone will come down with it. AMD is also more common in Caucasians than among African-Americans, Asians, or Hispanics. But the largest risk factor is age: the older you get, the more likely you are to be afflicted by AMD.