This file type includes high-resolution graphics and schematics when applicable.
When we think about simulation here at Machine Design, we usually dwell on testing parts for static or dynamic stress analysis. For engineers, simulation is a check system for the parts we produce,and on how well our mechanical component can endure a stress, deflection, or repeated cycle movement.
However, the simulation landscape is expanding and encroaching into newer technologies. The field of medicine, for example, is integrating computer aided design, modeling, and simulation to help doctors perform medical procedures. These CAD models and simulation are now essential to ensure proper surgery, recreation of models for training purposes, and prediction of how organs will perform.
Surgical Advances Using CAD Modeling
The planning process prior to surgery involves taking CT and MRI scans to accurately model the patientâs features. Then modeling is done using CAD to develop the plan for surgery and reconstructive features using either 3D-printed material, plastic, or metal. (Courtesy of Dr. Derek Steinbacher)
Dr. Derek Steinbacher is an expert on the use of virtual surgical planning in bone and soft-tissue analysis and procedures. Traditionally, surgical planning has been used on just bone manipulation, due to the modeling software not being able to accurately depict soft materials like cloth or skin. However, the software is now powerful enough to not only perform computer tomography (CT) based soft-tissue analysis, but goes beyond to three-dimensional digital photogrammetry to predict the fine details of soft-tissue dynamics for both pre- and post-operative settings.
Speaking with Dr. Steinbacher, he lists the many uses of CAD in surgery: “For the skeleton/bony movements, we can plan manipulations, osteotomies, resections, and reconstruction of the bone in space. Beginning first digitally/virtually, and then with 3D-printed splints or guides, help us with the bone cuts or positions, and printed plates or implants can be used intraoperatively for fixation or for parts of the reconstructions.”
The essential steps for surgical planning with computer-aided design are: analysis, planning, virtual surgery, implant design/production, and postoperative analysis. The first step of analysis is to understand the diagnosis and develop the solution. The initial data is a tomographic scan with the appropriate parameters. The raw CT data is converted to structure triangulation language format for digital modeling purposes. The linear, angular, and volumetric measurements are the overlays of normal anatomy. The doctors use the data to quantitatively understand the preoperative state of the patient’s structure.
Virtual surgery comes from the tomographic data. For example, defect reconstruction surgery is tried virtually first with appropriate size/contour material. A mirror image of the contralateral side guides the reconstruction surgery in a unilateral defect. The average anatomical overlay indicates the requirements of reconstruction. The magnitude and spatial positioning of the reconstructive surgery depends on present structures, quantitative parameters, and relationships to nearby anatomical intact structures. The pre-planning also takes into account factors of overcorrection, growth, and relapse. With the endpoints established, they initially perform the surgery digitally.
This image shows how pre-planning with CAD models occurs in bone skull operations. Image B1 is the three-dimensional plan performed using digital moldable âclay.â The material is shaped to fill the defect with the appropriate size, shape, and contour. B2 and B3 illustrate how the custom-fabricated milled titanium mesh offers protection and esthetic function. (Courtesy of Dr. Derek Steinbacher)
Using the CAD and simulation tools, the doctor attempts several different methods and strategies to determine the most optimal approach. The approaches consider comprehensive anatomical examination of the reconstruction, new location of repositioned bone (including the position of nearby vasculature/nerve features), and recognition of unanticipated consequences, collisions, and problems long before performing the actual procedure.
Designs for the treatment guides and implants occur once the virtual surgical planning is chosen. Fabricated biocompatible implants and splints use the digital information and the solution derived from the virtual surgery. These include multiple materials such as biocompatible/sterilization plastic, titanium, and additive-manufacturing materials like stereolithography, selective laser sintering, and direct metal laser sintering.
Only a small percentage of doctors use CAD for pre-operational analysis, though the benefits are clear. “The surgeon still needs a proper understanding and treatment plan—the computer and CAD cannot generate this. But if the plan is appropriate, then the use of 3D planning and CAD/CAM will help ensure the surgeon is as close as possible to achieving his/her desired result [and it limits or eliminates the number of intraoperative variables],” says Steinbacher.
Future Innovations for CAD in Medicine
When it comes to using advance engineering tools in surgery, 3D printing is already a common tool in medicine. According to Dr. Steinbacher, “we print [3D] items to use intraoperatively—temporary guides/splints to use intraoperatively for positioning and then removal, and permanent implants, plates, etc. can be printed to complete the reconstruction.” When it comes to virtual or augmented reality, Dr. Steinbacher reports that “Google Glass and Oculus Rift have been reported, but not in the mainstream in surgery yet.”
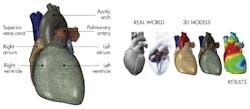
The Living Heart Projectâs goal is to provide accurate models of the heart for different areas of study. The models include a solid model, a finite-element model, a muscle-fiber model, and a fluid model. (Image courtesy of Simulia)
However, we do not have to wait long for virtual simulation to have a larger impact on medicine. Simulia and Dassault Systèmes are using simulation to help recreate the human heart. The Living Heart Project (LHP) is a joint effort led by cardiovascular researchers, educators, medical device developers, regulatory agencies, and practicing cardiologists to develop accurate personalized digital heart models. The five-year project started in 2014. The purpose of these models is to advance the training of future physicians, develop better medical devices, improve testing and clinical diagnosis, and assist in the future of regulatory science.
Users can view Living Heart Project models with a special set of 3D glasses and controllers for a close-up look. (Image courtesy of Simulia)
The LHP team utilizes Simulia Abaqus finite-element analysis as the primary software engine to create the virtual heart. Using data obtained from the CT and magnetic resonance imaging (MRI), the software creates an entire functioning heart including its four chambers (left and right ventricles and atria) and four valves (tricuspid, mitral, pulmonary, and aortic). Prior models only include a subset of the heart anatomy.
The team at LHP is able to create a more complex model. Taking into account a greater range of factors, they can model the interactions between electrical stimulation and mechanical contraction of muscle tissue. Irregularities between those factors may be the precursors to heart attacks or other heart dysfunctions.
The project develops a full of package models for different studies, including a solid model, a finite-element model, a muscle-fiber model, and a fluid model. The muscle fiber model accounts for the muscle sheets and fibers. The finite-element model simulates the mechanics of the heart, including the dynamic electrical behavior. Lastly, the fluid model provides insights into the flow, pressure, and other blood characteristics in the heart. The models are available to be manipulated via an augmented-reality headset and controllers. With these interface tools, physicians and researchers can interact with the different models.
Training with CAD and 3D-Printed Models
The most promising use case of CAD models is for training purposes. Dr. Saleem Abdulrauf, leading neurosurgeon-in-chief from St. Louis University Hospital, has found a prime test-case scenario for CAD-assisted medical training. Dr. Abdulrauf, who wants to tackle the complicated procedures of brain aneurysm surgery, explains, “I personally perform a lot of brain-aneurysm surgeries. It is a complex operation given the number of anatomical issues that we are dealing with under the microscope. I knew if there was a way of simulating those complications before the operation using the same tools and under the same microscope, we’d have a higher positive impact on the procedure outcome for the patient.”
His solution is to create an accurate high-resolution mapping of the patient’s brain into a 3D CAD model, similar to how the Living Heart Project creates models of the heart via CT and MRI scans. They create the model in real time from a current patient suffering from an aneurysm. The method would need to be quick and efficient, as the model would be a one-off part unique to each patient.
Prior to operating on a patientâs brain, Dr. Abdulrauf from St. Louis University Hospital, wants to see if practicing on a 3D-printed model would improve results and create less invasive surgery. (Courtesy of Todayâs Medical Developments site)
Stratasys Direct Manufacturing was chosen has the partner company to create polyjet brain models from the scans. Stratasys, working with St. Louis University, decided on PolyJet Rigid VeroYellow for the skull material and TangoPlus material with a durometer of Shore 27A for the brain. Within the 3D-printed brain was a version of the aneurysm.
By using these models, Dr. Abdulrauf is able to practice the surgery before performing the actual operation. According to Dr. Abdulrauf, “having the 3D-printed model here has a very positive impact on the procedure results. The model has helped to identify and overcome surgical challenges, like optimum access to the aneurysm or the depth and angle of the approach, before surgery begins.”
With initial positive results, Dr. Abdulrauf is performing a two-arm study where resident neurosurgeons practice on either a cadaver brain or a 3D-printed brain prior to performing actual brain-aneurysm operations. The accessors of the operations will not know which model the neurosurgeon practiced on prior to the actual surgery. This study will allow them to evaluate if practicing on realistic 3D CAD printed models enhanced the results of the surgery and help quantify the use of them in pre-surgical planning.
The world of computer-aided design is becoming more realistic with every technological step forward. As predicted by Dr. Steinbacher, the future of CAD, simulation, and virtual reality can provide “more accurate simulations; we wish to depict and predict how our surgical interventions will change the patient’s outcome and aesthetics (or reconstructed) anatomy accurately.” As we progress in creating more and more real-world-like models, the applications will expand not just for engineering, but into other fields as well.