3D-Printed Cell Traps Help Isolate Elusive Cancer Cells
A medical research team at the Georgia Institute of Technology quickly realized what many other cancer researchers knew: finding a handful of cancer cells among billions of blood cells in a patient sample is a daunting task. But the researchers had a new approach: They would use 3D-printed cell traps to remove white blood cells and filter out the red blood cells to leave only the tumor cells. This would let doctors diagnose patients with cancer early and advance the research into cancer metastasis. It would also let hospitals sequence the cancer cells to determine its specific type and then tailoring cancer treatment to the patient’s disease.
Other attempts to capture circulating tumor cells have tried extracting them from the blood using microfluidic technology that recognizes specific surface markers on cancer cells. But because the cancer can change over time, malignant cells can’t be recognized with certainty. And even if they are captured, the tumor cells must be removed from tiny, convoluted channels in the microfluidic device and separated from the antigen without causing damage.
The Georgia Tech team used 3D printing to build cell traps lined with antigens that could capture white blood cells in a sample. The let researchers greatly expand the surface area in the traps for capturing white blood cells as they pass by. Zig-zagging fluid channels, some as much as a half-meter long, increase the likelihood that every white blood cell would eventually contact a channel wall.
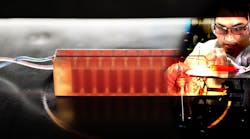
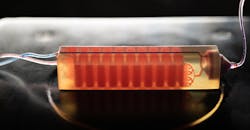
A 3D-printed cell trap developed in the lab of Georgia Tech captures blood cells to isolate tumor cells from a blood sample. (Photo: Allison Carter, Georgia Tech)
“Usual microfluidic devices have just a single layer with channels 50 to 100 microns,” says team leader A. Fatih Sarioglu, an assistant professor in Georgia Tech’s School of Electrical and Computer Engineering. “They are thick, but most of it just empty plastic. Using 3D printing liberates us from the single channel and lets us create many channels in three dimensions that better use the space.”
While 3D printing increased channel density, it also created an engineering challenge. Earlier microfluidic devices could have etched channels carrying the blood. But with 3D printing that fabricates structures layer-by-layer, channels had to be filled with wax to let more channels be built atop them. The torturous channel structure, designed to maximize cell-wall interaction, made it virtually impossible to remove the wax out after fabrication.
So the team ensured the cell traps would fit into standard centrifuges designed to spin samples for separation. Then traps could be heated in the centrifuge and spun to let melted wax escape. After removing the liquid wax, the channels were coated with the antigen.
After the white blood cells are removed, the smaller red blood cells pass through a simple commercial filter that traps cancer cells and any remaining white blood cells. The tumor cells are then removed from the filter, which is built into the 3D-printed trap.
A Georgia Tech researcher examines tumor cells captured using a 3D-printed cell trap. The trap captures white blood cells to isolate tumor cells from a blood sample. (Photo: Allison Carter, Georgia Tech)
One of the team’s goals is to develop an approach that requires as little processing of the blood samples as possible. This would make it easier for clinics and hospitals to analyze blood samples without needing technicians with specialized kills. Less processing also reduces the risk of damage to the tumor cells and minimizes other cellular changes that could interfere with the analysis.
To test their approach, the researchers coated white blood cells with biotin to accelerate testing. Future cell traps will use antigens that attract the cells to the channel walls without the biotin.
The researchers then added cancer cells to blood from healthy people. Because they knew how many cells were added, they could tell how many they should extract. The test showed the trap could capture around 90% of the tumor cells. Later testing of blood samples from prostate cancer patients isolated tumor cells from a 10-milliliter whole blood sample.
Testing included cells from prostate, breast, and ovarian cancer, but Sarioglu believes the device will capture circulating tumor cells from any type of cancer because the removal mechanism targets blood cells rather than cancer cells.
Next steps will be to narrow the channels in the device, test white blood cell removal without the use of biotin, boost the percentage of white cell extraction, and connect cell traps to increase trapping capacity.